Hand eczema is an inflammatory skin disorder, clinically characterized by redness, dry / cracked skin, swelling, and blisters. It may at times be complicated by bacterial infections, chiefly with Staphylococcus aureus. In addition to the hands, the wrists and the forearms are often involved. Hand eczema is common, with a 1-year prevalence of approximately 10% in the adult population
Hand eczema is typically a recurrent condition extending over years, and its appearance may vary over time. Redness, swelling and blisters are characteristic of acute eczema, whereas thicker, scaly skin with cracks are seen in chronic eczema. Hand eczema generally begins as acute eczema and then passes into a phase with chronic changes, sometimes with periods of acute eruptions. Important symptoms in hand eczema are itching and pain if there are fissures.
Identifiable Causes of Hand Eczema :
-
Significant exposure to irritants, for example wet work, intensive exposure to mineral oils, or friction
- Exposure to contact allergens in sensitized persons
- Exposure to proteins, for example occupational handling of foodstuffs
- Atopic constitution: atopic dermatitis and, less importantly, atopic mucous membrane symptoms
Skin contact with irritants
Skin contact with irritants can occur, for example, through wet work, intensive use of gloves, contact with mineral oils or organic solvents, and friction. These are known risk factors for hand eczema, especially among patients with atopic dermatitis. It is important that the exposures be described and quantified, as there is at present no other means of defining the diagnosis of irritant contact eczema.
Contact allergy detected by patch testing
Contact allergy detected by patch testing is a well-established cause of hand eczema in sensitized persons. This may be of particular significance in specific occupations. Contact allergy may also occur in private life and be related to leisure activities. Contact allergy is only a risk factor if there is ongoing or previous exposure of the hands to the allergen concerned.
Systemic allergic dermatitis (also referred to as ‘systemic contact dermatitis’) may appear as acute or recurrent vesicular hand eczema, if the patient ingests substantial amounts of a chemical substance or natural product for which the patient has a positive patch test reaction. The condition is rare, and, for example, the amount of nickel usually ingested in food does not trigger a reaction.
Skin contact with proteins
Skin contact with proteins, for example during occupational handling of foodstuffs, is also a well-known cause of hand eczema. Protein contact dermatitis may be underdiagnosed among exposed non-professionals. Contact reactions to proteins are typically of an urticarial type, and last from 0.5 to 2 hr. Characteristic symptoms among persons who react to foodstuffs are burning, stinging, and itching, seconds to minutes after contact with the foodstuff in question. Eczema may develop on repeated exposure. Protein contact may lead to eczema without a preceding urticarial reaction. The underlying immunological mechanisms are poorly elucidated. Immunoglobulin E (IgE) is undoubtedly involved in some reactions. Among patients with protein contact dermatitis, there is an overrepresentation of patients who had atopic dermatitis in childhood.
Atopic dermatitis
Atopic dermatitis in childhood and, less importantly, atopic mucous membrane symptoms are well-documented risk factors for the development of hand eczema in adulthood. Atopic dermatitis in childhood is also generally linked to a poor prognosis of hand eczema, with regard to both severity and duration. Filaggrin mutations may be of significance. Persons with atopic dermatitis probably have the same risk of contracting contact allergy as the background population.
Clinical types of Hand Eczema:
- Chronic fissured hand eczema
- Recurrent vesicular hand eczema
- Hyperkeratotic palmar eczema
- Pulpitis
- Interdigital eczema
- Nummular hand eczema
Chronic fissured hand eczema : This is defined as dry eczema, usually with scaling and possibly with hyperkeratotic areas and fissures, with a limited number of vesicles on the sides and palmar aspects of the fingers or on the palmar aspects of the hands. This morphology is typically seen in hand eczema that lasts from months to years.
Recurrent vesicular hand eczema: This is defined as recurrent eruptions of vesicles on the palms and/or on the sides of the fingers, and possibly also on the palmar aspects of the fingers and around the fingernails. Eruptions may occur at intervals of weeks or months. The eruptions may be so frequent that the eczema presents as chronic eczema. The eczema may also be present on the plantar aspects of the feet. The history of the patient gives information about the eruptive nature of this type of hand eczema.
Hyperkeratotic palmar eczema: This is defined as well-demarcated hyperkeratosis on the palms, possibly extending to the palmar aspects of the fingers. There may be fissures. This type of eczema is distinguished from psoriasis by not being inflammatory and by having no psoriasiform scaling. It does not evolve into psoriasis. There are no accompanying nail changes. There are no vesicles at any time. This eczema can also be seen on the plantar aspects of the feet. This type of eczema is most common among middle-aged men
Pulpitis: This is defined as hyperkeratotic eczema on the fingertips, possibly with fissures extending under the nails, especially on the thumbs and middle fingers, but it may affect all fingers; vesicles may occasionally be seen.
Interdigital eczema: This is defined as eczema in the proximal part of the interdigital spaces with erythema and scaling. Vesicles are rarely seen.
Nummular hand eczema: This is located on the dorsal aspects of the hands or fingers. The well-circumscribed lesions are characterized by erythema, keratosis, vesicles, and possibly oozing. Nummular eczema is frequently secondarily infected with S. aureus
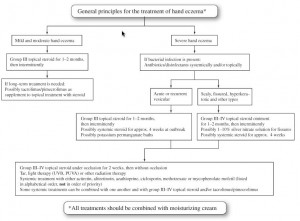 Treatment:
Treatment:
Menné et al, Contact Dermatitis Volume 65, Issue 1, pages 3–12, July 2011
